Homecare
Homecare is a service that allows patients to manage their care at home with the assistance of health care workers (such as nurses, physiotherapists, dietitians, personal support workers etc). It may be appropriate for you and your team to discuss whether you are eligible for homecare when planning for your discharge from hospital.
Homecare can provide a variety of services where appropriate, including: assistance with G-tubes, insulin injections, IV injections such as home IV antibiotics, wound care, and flushing/caring for central lines. They also provide home personal support for assistance with personal care, home physiotherapy, occupational therapy including home safety assessments, dietitian consultations, social work services, and speech language therapy services. They will also deliver some equipment to your home if needed. Homecare is also used for home palliation.
For more information, call the Home and Community Care Support Services (HCCSS) at:
Telephone: (416) 506-9888
Toll-free: (888) 470-2222
Website: https://healthcareathome.ca/
Managing Home Intravenous Antibiotics
Managing medications at home has advantages and disadvantages. In some cases, when you and your medical team feel that your condition is stable enough to continue your intravenous (IV) therapy at home, this option may be offered. However, this is not offered to all patients; it depends on your medical condition, your support at home, your comfort in managing home intravenous medications, availability of home care etc. More recently, homecare is also employing a “clinic first approach” and may require you to attend IV clinic appointments close to your house to help you initiate IV antibiotic therapy at home. As well, in order to qualify for home IV coverage you must have valid OHIP or private insurance or pre-approved coverage from your province of origin (this applies to out of province patients). If home IV is being arranged, your medical team will discuss:
- Antibiotic combinations compatible for the home
- Dosing schedule
- Duration of intravenous antibiotics
- Patient’s I.V. comfort and competence level
- Education surrounding mixing and infusing intravenous antibiotics
- Type of intravenous access (PICC, Port-a-cath) – see below for more information
- Preference of I.V. mode of delivery (Pump vs. gravity)
- Patient’s preference & life style
Arranging for Home Care can sometimes be a little complex and may require up to 3 days notice. Home Care (Home and Community Care Support Services – HCCSS) services can be affected by your date of discharge (weekend, holiday, etc.) and area of residence so if your team has agreed to home IV treatment please allow for this set up time. Ultimately, the decision for home treatment must be made by your team after talking with you. For more questions ask your CF team.

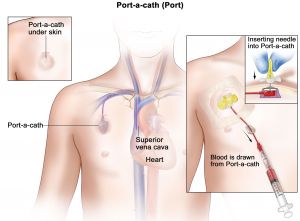 Your port-a-catheter device has one or two small reservoirs that are sealed with a soft silicone top, called a septum. The reservoir connects to a tube (a catheter) which is placed inside one of the large central veins that take blood to your heart. Once in place, your port device gives your care team “access” and medicine and fluids can be given through the needle.
Your port-a-catheter device has one or two small reservoirs that are sealed with a soft silicone top, called a septum. The reservoir connects to a tube (a catheter) which is placed inside one of the large central veins that take blood to your heart. Once in place, your port device gives your care team “access” and medicine and fluids can be given through the needle.